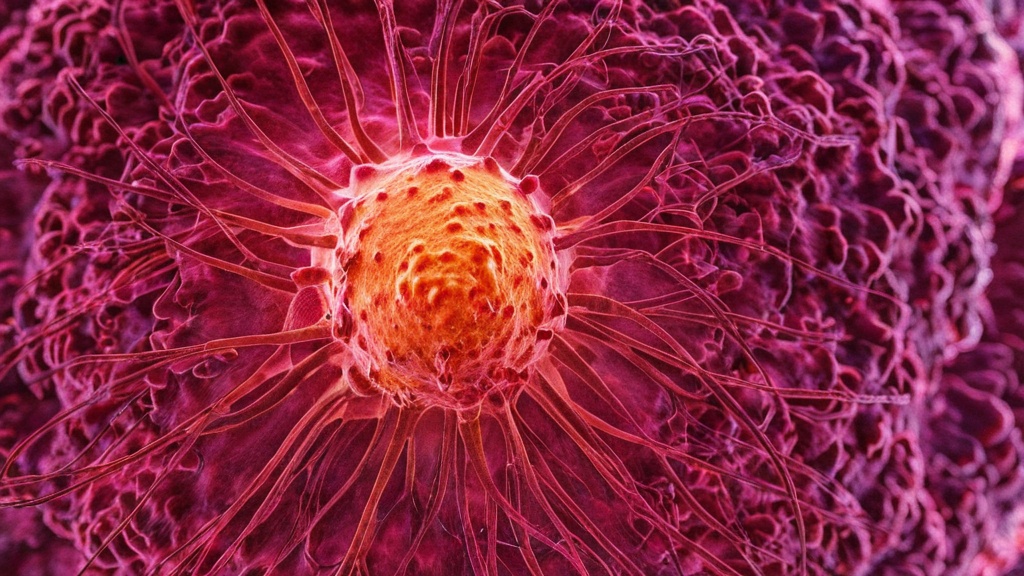
Human Papillomavirus (HPV) is a group of more than 200 related viruses. Some types of HPV can cause warts, while others can lead to cancer. HPV is the most common sexually transmitted infection worldwide. Most sexually active individuals will contract HPV at some point in their lives, often without realizing it.
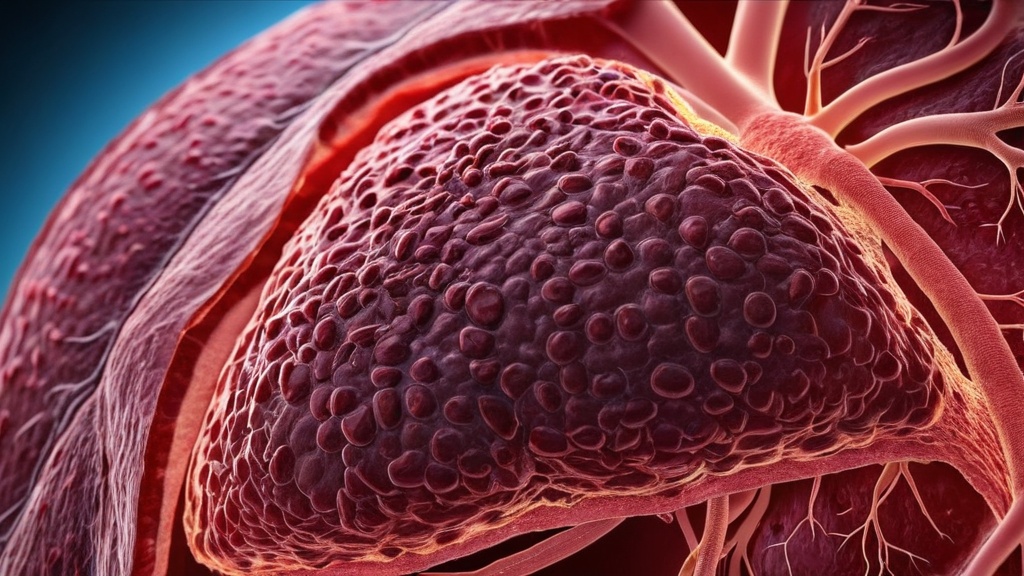
Cervical cancer is primarily caused by persistent infection with high-risk types of HPV, particularly HPV types 16 and 18. These strains are responsible for about 70% of cervical cancer cases. Understanding this connection is crucial for prevention and early detection strategies.
Not everyone with HPV will develop cervical cancer. Several risk factors can increase the likelihood of developing this disease. For instance, having multiple sexual partners or engaging in unprotected sex can elevate the risk of HPV infection. Additionally, a weakened immune system, whether due to HIV or other factors, can make it harder for the body to clear the virus.
Other factors include smoking and long-term use of birth control pills. Studies show that women who smoke are more likely to develop cervical cancer if they have HPV. Similarly, using hormonal contraceptives for five years or more may increase the risk of cervical cancer in women with HPV.
Vaccination against HPV is a powerful tool in preventing cervical cancer. The HPV vaccine protects against the most common high-risk types of the virus. It is most effective when given before individuals become sexually active, ideally between ages 11 and 12.
Research indicates that the vaccine significantly reduces the incidence of cervical pre-cancerous lesions. A study published in the Journal of Infectious Diseases found that vaccination led to a 90% reduction in HPV infections among vaccinated populations. This highlights the importance of widespread vaccination programs in reducing cervical cancer rates.
Most people with HPV do not experience any symptoms. In many cases, the immune system clears the virus naturally within two years. However, some individuals may develop genital warts or other health issues related to HPV.
Genital warts appear as small bumps or groups of bumps in the genital area. They can be raised or flat and may vary in size. If you notice any unusual growths or changes in your genital area, it’s essential to consult a healthcare provider for evaluation.
Regular Pap smears are vital for early detection of cervical cancer. A Pap smear involves collecting cells from the cervix to check for abnormalities that may indicate cancer or pre-cancerous changes. The American College of Obstetricians and Gynecologists recommends starting Pap tests at age 21, regardless of sexual history.
Women aged 21 to 29 should have Pap smears every three years. For those aged 30 to 65, a combination of Pap smear and HPV testing every five years is recommended. Early detection through regular screenings can significantly improve treatment outcomes and survival rates.
Lifestyle choices play a significant role in the risk of HPV infection and cervical cancer development. A healthy diet rich in fruits and vegetables can boost the immune system, helping the body fight off infections like HPV. Regular exercise also contributes to overall health and can reduce cancer risk.
Conversely, smoking and excessive alcohol consumption can weaken the immune system and increase cancer risk. A study published in Cancer Epidemiology, Biomarkers & Prevention found that women who smoke are at a higher risk for developing cervical cancer if they have HPV. Making healthier lifestyle choices can help lower these risks.
Protecting yourself from HPV involves several proactive steps. First, getting vaccinated against HPV is one of the most effective ways to prevent infection and subsequent cervical cancer.
Additionally, practicing safe sex by using condoms can reduce the risk of transmitting HPV, although it does not eliminate it entirely. Limiting the number of sexual partners can also decrease exposure to the virus. Regular health check-ups and screenings are essential for early detection and prevention.
Safe sexual practices are crucial in preventing HPV transmission. Using condoms consistently and correctly can lower the risk of contracting HPV and other sexually transmitted infections (STIs). While condoms do not provide complete protection against HPV, they significantly reduce transmission rates.
Communication with partners about sexual health is also vital. Discussing vaccination status and STI testing can help create a safer sexual environment. Educating oneself about safe practices empowers individuals to make informed decisions regarding their sexual health.
HPV testing plays a critical role in cervical cancer prevention strategies. This test detects the presence of high-risk HPV types that can lead to cervical cancer. It is often performed alongside a Pap smear for women aged 30 and older.
If high-risk HPV is detected, further monitoring or treatment may be necessary to prevent the development of cervical cancer. Research shows that combining Pap smears with HPV testing improves early detection rates, leading to better outcomes for women at risk.
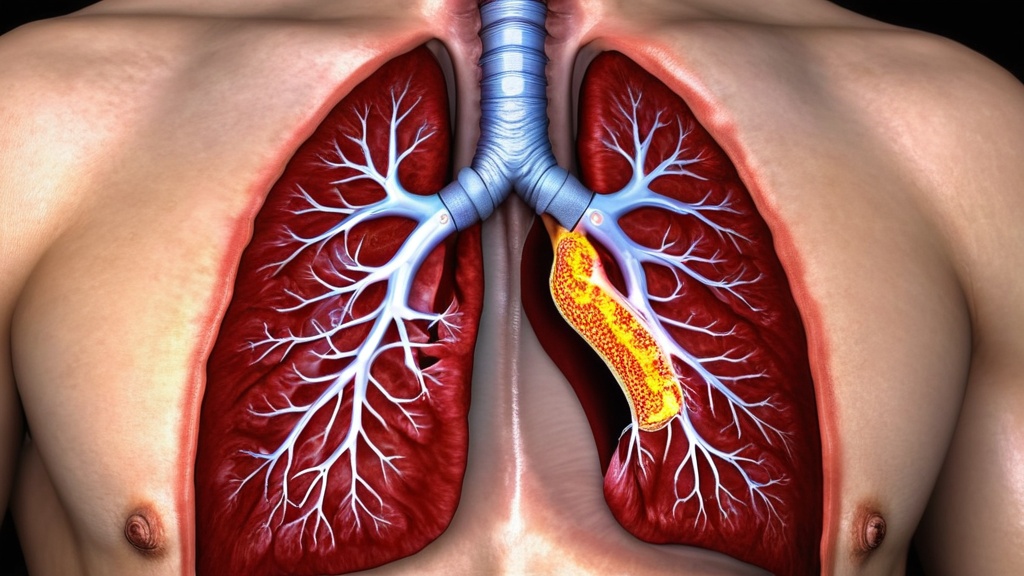
While HPV is most commonly associated with cervical cancer, it also links to several other cancers. These include anal, vulvar, vaginal, penile, and oropharyngeal cancers. High-risk types of HPV are responsible for approximately 90% of anal cancers and about 70% of oropharyngeal cancers.
Understanding this broader connection emphasizes the importance of vaccination and regular screenings for all individuals, not just those at risk for cervical cancer. Awareness can lead to earlier detection and better treatment options for various cancers associated with HPV.
Support is available for individuals affected by HPV and cervical cancer. Organizations like the American Cancer Society provide resources for education, support groups, and information on treatment options. They also offer guidance on navigating healthcare systems and understanding medical terminology.
Local health departments often provide free or low-cost screenings and vaccinations. Online communities can also offer emotional support and shared experiences from others facing similar challenges. Seeking out these resources can empower individuals to take charge of their health and well-being.
In conclusion, understanding HPV’s role in cervical cancer is essential for prevention and early detection strategies. By prioritizing vaccination, regular screenings, and healthy lifestyle choices, individuals can significantly reduce their risk of developing cervical cancer and other related health issues.
FAQs
What is the relationship between HPV and cervical cancer?
Human papillomavirus (HPV) is a group of viruses, some of which are high-risk types that can cause cervical cancer. Persistent infection with high-risk HPV types can lead to changes in cervical cells, which may develop into cancer over time.
How common is cervical cancer worldwide?
Cervical cancer is one of the most common cancers among women globally, particularly in low- and middle-income countries. It is estimated to be the fourth most frequent cancer in women worldwide.
Can cervical cancer be prevented?
Yes, cervical cancer can be largely prevented through regular screening (such as Pap smears and HPV testing), vaccination against HPV, and practicing safe sexual behaviors to reduce HPV transmission.
What are the symptoms of cervical cancer?
Early-stage cervical cancer often has no symptoms. When symptoms appear, they may include abnormal vaginal bleeding, pelvic pain, pain during intercourse, or unusual vaginal discharge.
Is there a vaccine available for HPV?
Yes, vaccines are available that protect against the most common high-risk HPV types responsible for cervical cancer. The HPV vaccine is recommended for preteens and young adults to reduce the risk of HPV infection and related cancers.